THE STORY BEHIND OUR DATA-VISUALISATION TOOL
If we don’t know how gender, and the systems and structures tied up with it, negatively impact our health, how can we make the changes needed for everyone to have an equal chance of living well?
At Global Health 50/50, we work closely with health and data professionals, policymakers and advocates, pushing together for gender equality in the global health landscape. We provide accessible, engaging evidence on the impacts of sex and gender on health and highlight successful policy approaches that turn evidence into action.
But we believe change needs to happen faster, and that the power of data should be open to everyone, so that countries and communities can identify ways to drive their own progress.
Where Pathways began
Our Gendered Health Pathways work started as COVID-19 swept the world. Over the course of the pandemic, we gathered, analysed and published data, disaggregated by sex and other characteristics, on testing, vaccination, hospitalisation and death. Our COVID-19 Tracker became the world’s largest repository of sex-disaggregated data, was used by multiple UN dashboards and covered widely in the national and global media.
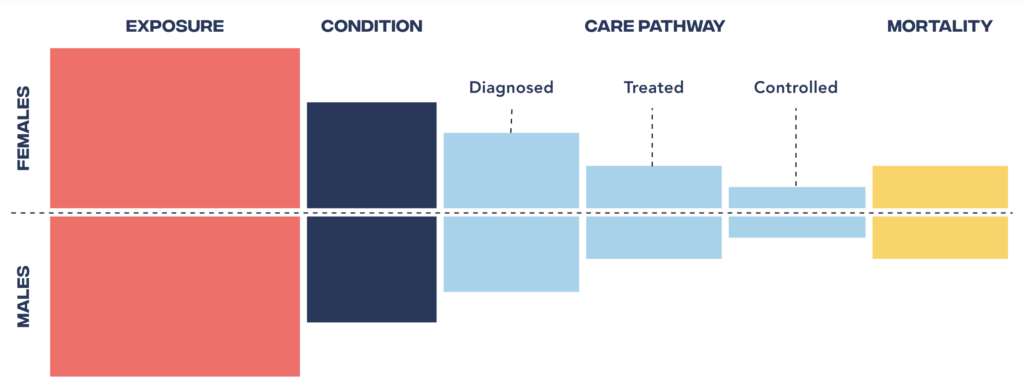
The work revealed some significant gender differences and raised important questions. For example, why were men less likely to get tested, but more likely to be hospitalised? And why didn’t women have the same access to intensive care as men?
Knowing that COVID-19 was not alone in its gendered drivers and impacts, we took the lessons learned from the COVID-19 Tracker work and expanded it to better understand gender differences across other life-threatening health conditions.
The result is Gendered Health Pathways, our breakthrough data visualisation tool.
HOW WE PLAN TO USE THE PATHWAYS
Ultimately Gendered Health Pathways is a tool for anyone who wants to help change lives for the better.
As a proof-of-concept, there’s huge potential for using and developing the Pathways tool at country and global levels. And we’ve already begun partnering with ministries of health and public health schools to use and adapt it using their own data-sets.
Equally, it has the potential to empower communities at the grassroots to drive change for the people and causes they represent. Help us realise the full potential of Gendered Health Pathways — and with it, better health and wellbeing for all. Read on to find out more about our plans to use and develop the Pathways.
FAQS
Got a question about Gendered Health Pathways? Explore the common queries below to find out more about the data and thinking behind it, and how the tool can be utilised by advocates, policymakers and researchers to improve the health of women, men and non-binary people worldwide.
As Gendered Health Pathways evolves, we welcome ongoing engagement with those using it, whether in the global health community or beyond, so we can further strengthen its impact and ensure its relevance for future policymaking and research. Read on to find out more.
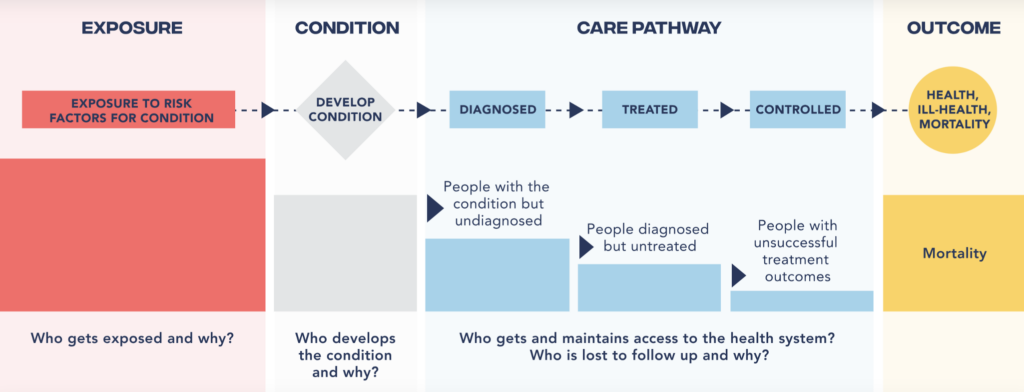
What is the ‘health pathway’?
The health pathway is a framework that connects a series of steps along a person’s health journey — from risk exposure to disease diagnosis, treatment, and control as well as prevalence and death. It brings together data on each step and thereby helps us identify who is being left behind at what step of the pathway and where gaps in policies, responses, and care need to be addressed.
Where does the data come from?
The data presented in this visualisation comes from leading global health organisations and data providers, including the World Health Organization’s STEPS surveys, UNAIDS, the Global Burden of Disease project from the Institutes for Health Metrics and Evaluation (IHME), and the NCD-RisC collaboration.
We’ve carefully sourced data on risk factors, care cascades, and disease outcomes, disaggregated by sex and age, to provide a comprehensive view of the gendered health pathways for diabetes, hypertension, and HIV.
Why are there differences in data availability for different countries?
Differences in data availability and quality between countries are a reality in global health. Some countries have more robust data collection systems, while others face challenges in gathering and publishing disaggregated globally comparable data. Other countries choose not to share their data for inclusion in global datasets. We are constantly working to improve the breadth and depth of our data, including by collaborating with country-level health agencies and other organisations.
Why does the tool focus on diabetes, hypertension, and HIV, and not other conditions?
We present these three conditions because they are among the leading causes of death and disability worldwide, and crucially, these were the only three conditions — thus far — where we were able to find globally comparable data that is disaggregated by sex and age along the health pathway.
Our intention is to work with others in the global health community to build more pathways for more conditions, and realise the tool’s full potential to promote gender-responsive policies and practices. Find out more
Why do you focus on sex and gender differences in health pathways?
Sex and gender are key determinants of health. They influence everything from risk factors to health-related behaviours, healthcare access and treatment outcomes. Focusing on these differences is crucial for understanding health disparities and for developing strategies to address them effectively.
Some of the differences we see in health outcomes are due to sex (the biological factors that influence genetic make-up and bodily systems). Sex interacts with gender (the systems and structures of society that influence norms, behaviours and the distribution of power according to gender identity) in driving health outcomes. Gender influences rates of risk exposure (such as the likelihood of living in poverty, or the likelihood of working in polluted conditions), health behaviours (such as social norms influencing who smokes tobacco or who drinks alcohol), and a person’s interaction with the health system (such as the likelihood of receiving quality services). These factors collectively impact health outcomes for everyone, including women, men, and non-binary people.
This is why collecting and analysing sex-disaggregated data is so important — it helps us identify where interventions are needed to improve health outcomes across all gender identities.
How are the terms sex and gender used?
Why sex AND gender? Sex generally refers to biological sex and is usually categorised as female or male. Gender refers to the socially constructed roles, behaviours, expressions and identities of girls, women, boys, men, and gender-diverse people.
National surveillance systems are not globally consistent in whether they capture assigned sex at birth or gender identity, which may be different for a person, in their health surveys. Therefore we use ‘sex/gender’ in most cases in recognition of both approaches.
Why does the visualisation only focus on men and women; what about non-binary and transgender health pathways?
The concept of the health pathway lends itself to any range of disaggregated population groups, but relies on the availability of globally comparable national datasets. We were only able to find and visualise data in a binary way (male/female). We acknowledge that this does not fully capture the diversity of gender identities, but we’re limited to what is currently collected and reported by countries.
We’re committed to addressing this gap in future iterations of the tool — if and when more inclusive data becomes available.
Why do you list only three to five risk factors for each condition?
The health pathways are designed to highlight the most significant and impactful risk factors for each condition. While there are certainly more factors that can influence health outcomes, focusing on the most prominent risk factors ensures that the visualisation remains clear and actionable for policymakers, healthcare providers, and advocates.
How frequently is the data updated?
The data is updated as frequently as new, validated information becomes available from our sources. We work with the best available datasets, but it’s important to acknowledge that some datasets may have delays due to the nature of global health data publication.
The most recent datasets, which are currently visualised, are from: Risk factors (IHME, 2019); HIV diagnosis, treatment, control (UNAIDS, XX), Hypertension diagnosis, treatment, control ( XX), Diabetes diagnosis, treatment, control (NCD-STEPS Survey, XX), prevalence and mortality for all conditions (IHME, 2019).
Can I download the data?
Currently, the data is presented through our interactive platform. While we don’t offer direct data downloads right now, we encourage you to get in touch if you need specific data points or are interested in collaborating to expand the accessibility of this data.
How can Gendered Health Pathways help policy makers, health professionals and researchers address global health inequalities?
Gendered Health Pathways is a valuable resource for policy-makers, public health and healthcare professionals, and researchers seeking to understand the role of gender in health outcomes. By revealing where inequalities persist across the health pathway between women and men, we can make the case for specific targeted interventions, highlight underserved populations, and push for policies and practices that ensure better health outcomes for all.
Does the Gendered Health Pathways tool include any data on the intersection of gender with other social determinants of health?
While the tool primarily focuses on gender and health, we recognise that other factors, such as socioeconomic status, race, and geography, also significantly impact health outcomes. Expanding the dataset to include these intersections is a priority for future updates.
We’re actively seeking funding and sponsorship to make this expansion possible. If you are interested in supporting this important work, please reach out to us.
Will the Gendered Health Pathways tool be updated to reflect new data or emerging health issues?
We hope to periodically update the tool to reflect the latest data on health risk factors, the care cascade, and outcomes. As new health challenges emerge, we hope to incorporate them into the pathways to keep the tool accurate and relevant. Additionally, as globally comparable datasets become available, they could be added to further enhance the tool.
However, updates rely on the availability of robust data as well as securing the necessary funding and resources. We are actively seeking support to make this possible. If you are interested in contributing to this important work, please don’t hesitate to reach out to us.
Can the Gendered Health Pathways tool be used for educational purposes?
Yes! Gendered Health Pathways and its data visualisation dashboard can be a powerful educational tool for students, healthcare professionals, and advocates — in many ways. It can be used to teach about the intersections of gender, health, and policy, and help learners understand how societal factors shape health outcomes.
Can I contribute to the development of this initiative? If so, how?
Yes, we’re always looking for new insights, collaborators, and experts who can help us expand, enhance and improve the impact of the Gendered Health Pathways programme.
You can contact us by sending us a message on our website. We’re happy to discuss the initiative, answer questions, and collaborate with other organisations working towards gender justice in health.
Only through collaboration will we realise its full potential in promoting gender-responsive policies and practices.
PATHWAY STORIES

What can we learn when we look more closely at the deeply rooted differences dividing men’s and women’s journeys along the health pathway — from exposure to risks to rate of survival.
TAKE ACTION